Contents
Fertility is the ability to conceive a child. The fertility rate is the average number of children born during an individual's lifetime and is quantified demographically. Conversely, infertility is the difficulty or inability to reproduce naturally. In general, infertility is defined as not being able to conceive a child after one year (or longer) of unprotected sex.[1] Because infertility is widespread, fertility specialists all over the world assist persons and couples who experience difficulties conceiving a baby.
Fertility is an issue for people of both sexes. According to the Centers for Disease Control and Prevention, in 35% of couples who cannot conceive, the cause can be attributed to factors on both the female and male side.[1] Human fertility depends on various factors including nutrition, sexual behaviour, consanguinity, culture, instinct, endocrinology, timing of conception, economics, personality,[2] lifestyle, and emotions.
Fertility differs from fecundity, which is defined as the biological capacity to reproduce irrespective of intention for conception.[3] Fecundity can be explained by gamete production, fertilization, and carrying a pregnancy to term.[4] The antithesis of fertility is infertility, while the antithesis of fecundity is sterility.
Demography
In demographic contexts, fertility refers to the actual production of offspring, rather than the physical capability to produce which is termed fecundity.[5][6] While fertility can be measured, fecundity cannot be. Demographers measure the fertility rate in a variety of ways, which can be broadly broken into "period" measures and "cohort" measures. "Period" measures refer to a cross-section of the population in one year. "Cohort" data on the other hand, follows the same people over a period of decades. Both period and cohort measures are widely used.[7]
Period measures
- Crude birth rate (CBR) - the number of live births in a given year per 1,000 people alive at the middle of that year. One disadvantage of this indicator is that it is influenced by the age structure of the population.
- General fertility rate (GFR) - the number of births in a year divided by the number of women aged 15–44, times 1000. It focuses on the potential mothers only, and takes the age distribution into account.
- Child-Woman Ratio (CWR) - the ratio of the number of children under 5 to the number of women 15–49, times 1000. It is especially useful in historical data as it does not require counting births. This measure is actually a hybrid, because it involves deaths as well as births. (That is, because of infant mortality some of the births are not included; and because of adult mortality, some of the women who gave birth are not counted either.)
- Coale's Index of Fertility - a special device used in historical research
Cohort measures
- Total fertility rate (TFR) - the total number of children a woman would bear during her lifetime if she were to experience the prevailing age-specific fertility rates of women. TFR equals the sum for all age groups of 5 times each ASFR rate.[8]
- Gross Reproduction Rate (GRR) - the number of girl babies a synthetic cohort will have. It assumes that all of the baby girls will grow up and live to at least age 50.
- Net Reproduction Rate (NRR) - the NRR starts with the GRR and adds the realistic assumption that some of the women will die before age 49; therefore they will not be alive to bear some of the potential babies that were counted in the GRR. NRR is always lower than GRR, but in countries where mortality is very low, almost all the baby girls grow up to be potential mothers, and the NRR is practically the same as GRR. In countries with high mortality, NRR can be as low as 70% of GRR. When NRR = 1.0, each generation of 1000 baby girls grows up and gives birth to exactly 1000 girls. When NRR is less than one, each generation is smaller than the previous one. When NRR is greater than 1 each generation is larger than the one before. NRR is a measure of the long-term future potential for growth, but it usually is different from the current population growth rate.
Social and economic determinants of fertility
A parent's number of children strongly correlates with the number of children that each person in the next generation will eventually have.[9] Factors generally associated with increased fertility include religiosity,[10] intention to have children,[11] and maternal support.[12] Factors generally associated with decreased fertility include wealth, education,[13][14] female labor participation,[15] urban residence,[16] cost of housing,[17][18] intelligence, increased female age and (to a lesser degree) increased male age.
The "Three-step Analysis" of the fertility process was introduced by Kingsley Davis and Judith Blake in 1956 and makes use of three proximate determinants:[19][20] The economic analysis of fertility is part of household economics, a field that has grown out of the New Home Economics. Influential economic analyses of fertility include Becker (1960),[21] Mincer (1963),[22] and Easterlin (1969).[23] The latter developed the Easterlin hypothesis to account for the Baby Boom.
Bongaarts' model of components of fertility
Bongaarts proposed a model where the total fertility rate of a population can be calculated from four proximate determinants and the total fecundity (TF). The index of marriage (Cm), the index of contraception (Cc), the index of induced abortion (Ca) and the index of postpartum infecundability (Ci). These indices range from 0 to 1. The higher the index, the higher it will make the TFR, for example a population where there are no induced abortions would have a Ca of 1, but a country where everybody used infallible contraception would have a Cc of 0.
TFR = TF × Cm × Ci × Ca × Cc
These four indices can also be used to calculate the total marital fertility (TMFR) and the total natural fertility (TN).
TFR = TMFR × Cm
TMFR = TN × Cc × Ca
TN = TF × Ci
- Intercourse
- The first step is sexual intercourse, and an examination of the average age at first intercourse, the average frequency outside marriage, and the average frequency inside.
- Conception
- Certain physical conditions may make it impossible for a woman to conceive. This is called "involuntary infecundity." If the woman has a condition making it possible, but unlikely to conceive, this is termed "subfecundity." Venereal diseases (especially gonorrhea, syphilis, and chlamydia) are common causes. Nutrition is a factor as well: women with less than 20% body fat may be subfecund, a factor of concern for athletes and people susceptible to anorexia. Demographer Ruth Frisch has argued that "It takes 50,000 calories to make a baby". There is also subfecundity in the weeks following childbirth, and this can be prolonged for a year or more through breastfeeding. A furious political debate raged in the 1980s over the ethics of baby food companies marketing infant formula in developing countries. A large industry has developed to deal with subfecundity in women and men. An equally large industry has emerged to provide contraceptive devices designed to prevent conception. Their effectiveness in use varies. On average, 85% of married couples using no contraception will have a pregnancy in one year. The rate drops to the 20% range when using withdrawal, vaginal sponges, or spermicides. (This assumes the partners never forget to use the contraceptive.) The rate drops to only 2 or 3% when using the pill or an IUD, and drops to near 0% for implants and 0% for tubal ligation (sterilization) of the woman, or a vasectomy for the man.
- Gestation
- After a fetus is conceived, it may or may not survive to birth. "Involuntary fetal mortality" involves natural abortion, miscarriages and stillbirth (a fetus born dead). Human intervention intentionally causing abortion of the fetus is called "therapeutic abortion".
Fertility biology
Women have hormonal cycles which determine when they can achieve pregnancy. The cycle is approximately twenty-eight days long, with a fertile period of five days per cycle, but can deviate greatly from this norm. Men are fertile continuously, but their sperm quality is affected by their health, frequency of ejaculation, and environmental factors.[24]
Fertility declines with age in both sexes. For women, the decline begins around the age of 32, and becomes precipitous at age 37. For men, potency and sperm quality begins to decline around the age of 40. Even if an older couple does manage to conceive a child, the pregnancy will be increasingly difficult for the mother, and carries a higher risk of birth defects and genetic disorders for the child.[25]
Pregnancy rates for sexual intercourse are highest when it occurs every 1 or 2 days,[26] or every 2 or 3 days.[27] Studies have found no significant difference between different sex positions and pregnancy rate, as long as it results in ejaculation into the vagina.[28]
Menstrual cycle
A woman's menstrual cycle begins, as arbitrarily assigned, with menses. Next is the follicular phase where estrogen levels build as an ovum matures (due to the follicular stimulating hormone, or FSH) within the ovary. When estrogen levels peak, it spurs a surge of luteinizing hormone (LH) which completes maturation and enables the ovum to break through the ovary wall.[30] This is ovulation. During the luteal phase following ovulation LH and FSH cause the post-ovulation ovary to develop into the corpus luteum which produces progesterone. The production of progesterone inhibits the LH and FSH hormones which (in a cycle without pregnancy) causes the corpus luteum to atrophy, and menses to begin the cycle again.
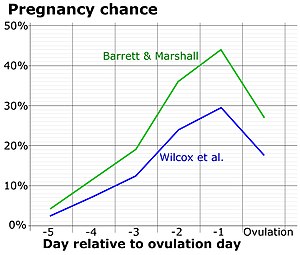
Peak fertility occurs during just a few days of the cycle: usually two days before and two days after the ovulation date.[31] This fertile window varies from woman to woman, just as the ovulation date often varies from cycle to cycle for the same woman.[32] The ovule is usually capable of being fertilized for up to 48 hours after it is released from the ovary. Sperm survive inside the uterus between 48 and 72 hours on average, with the maximum being 120 hours (5 days).
These periods and intervals are important factors for couples using the rhythm method of contraception.
Female fertility
The average age of menarche in the United States is about 12.5 years.[33] In postmenarchal girls, about 80% of the cycles are anovulatory (ovulation does not actually take place) in the first year after menarche, 50% in the third and 10% in the sixth year.[34]
Menopause occurs during a woman's midlife between ages 48 and 55.[35][36] During menopause, hormonal production by the ovaries is reduced, eventually causing a permanent cessation of the creation of the uterine lining (period). This is considered the end of the fertile phase of a woman's life.
The predicted effect of age on female fertility in women trying to get pregnant, without using fertility drugs or in vitro fertilization:[37]
- At age 30
- 75% will conceive ending in a live birth within one year
- 91% will conceive ending in a live birth within four years.
- At age 35
- 66% will conceive ending in a live birth within one year
- 84% will conceive ending in a live birth within four years.
- At age 40
- 44% will conceive ending in a live birth within one year
- 64% will conceive ending in a live birth within four years.
Studies of couples trying to conceive have yielded better results: one 2004 study of 770 European women found that 82% of 35- to 39-year-old women conceived within a year,[38] while a study in 2013 of 2,820 Danish women saw 78% of 35- to 40-year-olds conceive within a year.[39]
According to an opinion by the Practice Committee of the American Society for Reproductive Medicine, specific coital timing or position, and resting supine after intercourse have no significant impact on fertility. Sperm can be found in the cervical canal seconds after ejaculation, regardless of coital position.[40]
Successful pregnancies facilitated by fertility treatment have been documented in women as old as 67.[41]
Male fertility
Some research suggests that older males have decreased semen volume, sperm motility, and impaired sperm morphology.[42] In studies that controlled for female partner's age, comparisons between men under 30 and men over 50 found relative decreases in pregnancy rates between 23% and 38%.[42] Sperm count declines with age, with men aged 50–80 years producing sperm at an average rate of 75% compared with men aged 20–50 years and larger differences exist in the number of seminiferous tubules in the testes containing mature sperm:[42]
- In males 20–39 years old, 90% of the seminiferous tubules contain mature sperm.
- In males 40–69 years old, 50% of the seminiferous tubules contain mature sperm.
- In males 80 years old and older, 10% of the seminiferous tubules contain mature sperm.[43]
Decline in male fertility is influenced by many factors, including lifestyle, environment and psychological factors.[44]
Some research suggests increased risks for health problems for children of older fathers, but no clear association has been proven.[45] A large scale study in Israel suggested that the children of men 40 or older were 5.75 times more likely than children of men under 30 to have an autism spectrum disorder, controlling for year of birth, socioeconomic status, and maternal age.[46] Increased paternal age has been suggested to correlate with schizophrenia but it is unproven.[47][48][49][50][51]
Australian researchers have found evidence to suggest obesity may cause subtle damage to sperm and prevent a healthy pregnancy. They reported fertilization was 40% less successful when the father was overweight.[52]
The American Fertility Society recommends an age limit for sperm donors of 50 years or less,[53] and many fertility clinics in the United Kingdom will not accept donations from men over 40 or 45 years of age.[54]
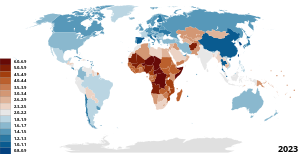
Historical trends by country
France
The French pronatalist movement from 1919 to 1945 failed to convince French couples they had a patriotic duty to help increase their country's birthrate. Even the government was reluctant in its support to the movement. It was only between 1938 and 1939 that the French government became directly and permanently involved in the pronatalist effort. Although the birthrate started to surge in late 1941, the trend was not sustained. Falling birthrate once again became a major concern among demographers and government officials beginning in the 1970s.[55] In mid-2018, there was a bill introduced to legalize single women and lesbian couples to get fertility treatment. At the beginning of 2020, the Senate approved the bill 160 votes to 116. They are a step closer to legalizing fertility treatments for all women regardless of sexual orientation or marital status. Soon there will be no reason for lesbian couples or single women to travel to be able to start their own family.[56]
Korea

South Korea has the lowest fertility rate in the world at 0.78.[57] A variety of explanations have been proposed, ranging from investment in education[58] to birth control, abortion, a decline in the marriage rate, divorce, female participation in the labor force, and the 1997 Asian financial crisis.[59] After being legal from the 1960s to the 1980s, abortion was again made illegal in South Korea in the early 2000s in an attempt to reverse the declining fertility rate.[60]
United States

From 1800 to 1940, fertility fell in the US. There was a marked decline in fertility in the early 1900s, associated with improved contraceptives, greater access to contraceptives and sexuality information and the "first" sexual revolution in the 1920s.
Post-WWII
After 1940 fertility suddenly started going up again, reaching a new peak in 1957. After 1960, fertility started declining rapidly. In the Baby Boom years (1946–1964), women married earlier and had their babies sooner; the number of children born to mothers after age 35 did not increase.[62]
Sexual revolution
After 1960, new methods of contraception became available, ideal family size fell, from 3 to 2 children. Couples postponed marriage and first births, and they sharply reduced the number of third and fourth births.[63]
Impact of external factors on fertility
Studies have been conducted to identify external factors that impact fertility rates and embryo development. Two main factors were determined to have the greatest impact, eating habits and lifestyle choices.[64] Eating choices include quality, types and frequency of food intake. Grains, fruits and vegetables have a positive influence on embryo quality. Alcohol intake, cigarette and marijuana use all have a detrimental impact on female reproductive function.[65] During embryogenesis, the DNA structure and expression can be heavily influenced by lifestyle, nutrition and environmental toxins.[66]
Infertility
Infertility primarily refers to the biological inability of a person to contribute to conception. Infertility may also refer to the state of a woman who is unable to carry a pregnancy to full term. There are many biological causes of infertility, including some that medical intervention can treat.[67]
See also
- Anti-natalism
- Birth control
- Family economics
- Family planning
- Fecundity
- Fertility clinic
- Fertility tourism
- Fertility deity
- Fertility preservation
- Human Fertilisation and Embryology Authority
- Natalism
- Natural fertility
- Oncofertility
- Reproductive health
- Sub-replacement fertility
- Total fertility rate
- Vasectomy
- Fertility-development controversy
- Fertility factor (demography)
Further reading
- Bloom, David E.; Kuhn, Michael; Prettner, Klaus (2024). "Fertility in High-Income Countries: Trends, Patterns, Determinants, and Consequences". Annual Review of Economics.
References
- ^ a b "Infertility | Reproductive Health | CDC". www.cdc.gov. 2022-03-03. Retrieved 2023-03-02.
- ^ Skirbekk V, Blekesaune M (2014) [2014]. "Personality Traits Increasingly Important for Male Fertility: Evidence from Norway". European Journal of Personality. 28 (6): 521–529. doi:10.1002/per.1936. ISSN 0890-2070. S2CID 143134400.
- ^ Smarr MM, Sapra KJ, Gemmill A, Kahn LG, Wise LA, Lynch CD, et al. (March 2017). "Is human fecundity changing? A discussion of research and data gaps precluding us from having an answer". Human Reproduction. 32 (3): 499–504. doi:10.1093/humrep/dew361. PMC 5850610. PMID 28137753.
- ^ Schultz PT (June 1976). "Fertility Determinants: A Theory, Evidence, and an Application to Policy Evaluation". Population and Development Review. 2 (2): 293. doi:10.2307/1972043. JSTOR 1972043.
- ^ Frank O (27 September 2017). "The demography of fertility and infertility". www.gfmer.ch.
- ^ Last JM. "Fecundity and Fertility". Encyclopedia of Public Health. Archived from the original on 11 August 2009 – via enotes.com.
- ^ For detailed discussions of each measure see Paul George Demeny and Geoffrey McNicoll, Encyclopedia of Population (2003)
- ^ Another way of doing it is to add up the ASFR for age 10-14, 15-19, 20-24, etc., and multiply by 5 (to cover the 5 year interval).
- ^ Murphy M (3 July 2013). "Cross-national patterns of intergenerational continuities in childbearing in developed countries". Biodemography and Social Biology. 59 (2): 101–126. doi:10.1080/19485565.2013.833779. PMC 4160295. PMID 24215254.
- ^ Hayford SR, Morgan SP (1 March 2008). "Religiosity and Fertility in the United States: The Role of Fertility Intentions". Social Forces; A Scientific Medium of Social Study and Interpretation. 86 (3): 1163–1188. doi:10.1353/sof.0.0000. PMC 2723861. PMID 19672317.
- ^ Dommermuth L, Klobas J, Lappegård T (2014). Differences in childbearing by time frame of fertility intention. A study using survey and register data from Norway (Report). hdl:10419/192763.
- ^ Schaffnit SB, Sear R (1 July 2014). "Wealth modifies relationships between kin and women's fertility in high-income countries". Behavioral Ecology. 25 (4): 834–842. doi:10.1093/beheco/aru059.
- ^ Rai PK, Pareek S, Joshi H (1 January 2013). "Regression Analysis of Collinear Data using r-k Class Estimator: Socio-Economic and Demographic Factors Affecting the Total Fertility Rate (TFR) in India". Journal of Data Science. 11 (2): 323–342. doi:10.6339/JDS.2013.11(2).1030.
- ^ "Health and Education". Project Drawdown. 2020-02-12. Retrieved 2020-12-04.
- ^ Bloom D, Canning D, Fink G, Finlay J (2009). "Fertility, female labor force participation, and the demographic dividend". Journal of Economic Growth. 14 (2): 79–101. doi:10.1007/s10887-009-9039-9.
- ^ Sato Y (March 2007). "Economic geography, fertility and migration". Journal of Urban Economics. 61 (2): 372–387. doi:10.1016/j.jue.2006.08.002.
- ^ Li A (November 2019). "Fertility intention-induced relocation: The mediating role of housing markets". Population, Space and Place. 25 (8). doi:10.1002/psp.2265. hdl:11343/286897. S2CID 200012816.
- ^ Atalay K, Li A, Whelan S (25 June 2021). "Housing wealth, fertility intentions and fertility". Journal of Housing Economics. 54: 101787. doi:10.1016/j.jhe.2021.101787. S2CID 237787783.
- ^ Bongaarts J (March 1978). "A Framework for Analyzing the Proximate Determinants of Fertility". Population and Development Review. 4 (1): 105–132. doi:10.2307/1972149. JSTOR 1972149. S2CID 27026630.
- ^ Stover J (September 1998). "Revising the proximate determinants of fertility framework: what have we learned in the past 20 years?". Studies in Family Planning. 29 (3): 255–267. doi:10.2307/172272. JSTOR 172272. PMID 9789319.
- ^ Becker GS (1960). An Economic Analysis of Fertility. National Bureau Committee for Economic Research, Demographic and Economic Change in Developed Countries, a Conference of the Universities. Princeton, N.J.: Princeton University Press.
- ^ Mincer J (1963). "Market Prices, Opportunity Costs, and Income Effects". In Christ C (ed.). Measurement in Economics. Stanford, CA: Stanford University Press.
- ^ Easterlin RA (March 1975). "An economic framework for fertility analysis". Studies in Family Planning. 6 (3): 54–63. doi:10.2307/1964934. JSTOR 1964934. PMID 1118873.
- ^ Skakkebæk NE, Lindahl-Jacobsen R, Levine H, Andersson AM, Jørgensen N, Main KM, et al. (March 2022). "Environmental factors in declining human fertility". Nature Reviews. Endocrinology. 18 (3): 139–157. doi:10.1038/s41574-021-00598-8. PMID 34912078. S2CID 245134205.
- ^ George K, Kamath MS (September 2010). "Fertility and age". Journal of Human Reproductive Sciences. 3 (3): 121–123. doi:10.4103/0974-1208.74152. PMC 3017326. PMID 21234171.
- ^ "How to get pregnant". Mayo Clinic. 2016-11-02. Retrieved 2018-02-16.
- ^ "Fertility problems: assessment and treatment, Clinical guideline [CG156]". National Institute for Health and Care Excellence. 20 February 2013. Retrieved 2018-02-16. publication date: February 2013. last updated: September 2017
- ^ Imler PB, Wilbanks D. "The Essential Guide to Getting Pregnant" (PDF). American Pregnancy Association. Archived from the original (PDF) on 2018-06-01. Retrieved 2018-02-16.
- ^ Dunson DB, Baird DD, Wilcox AJ, Weinberg CR (July 1999). "Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation". Human Reproduction. 14 (7): 1835–1839. doi:10.1093/humrep/14.7.1835. PMID 10402400.
- ^ Danilovich N, Babu PS, Xing W, Gerdes M, Krishnamurthy H, Sairam MR (November 2000). "Estrogen deficiency, obesity, and skeletal abnormalities in follicle-stimulating hormone receptor knockout (FORKO) female mice". Endocrinology. 141 (11): 4295–4308. doi:10.1210/endo.141.11.7765. PMID 11089565.
- ^ "My Fertile Period | DuoFertility". Archived from the original on 2008-12-21. Retrieved 2008-09-22.
- ^ Creinin MD, Keverline S, Meyn LA (October 2004). "How regular is regular? An analysis of menstrual cycle regularity". Contraception. 70 (4): 289–292. doi:10.1016/j.contraception.2004.04.012. PMID 15451332.
- ^ Anderson SE, Dallal GE, Must A (April 2003). "Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart". Pediatrics. 111 (4 Pt 1): 844–850. doi:10.1542/peds.111.4.844. PMID 12671122.
- ^ Apter D (February 1980). "Serum steroids and pituitary hormones in female puberty: a partly longitudinal study". Clinical Endocrinology. 12 (2): 107–120. doi:10.1111/j.1365-2265.1980.tb02125.x. PMID 6249519. S2CID 19913395.
- ^ Takahashi TA, Johnson KM (May 2015). "Menopause". The Medical Clinics of North America. 99 (3): 521–534. doi:10.1016/j.mcna.2015.01.006. PMID 25841598.
- ^ Bourgeois JF, Gehrig PA, Veljovich DS (1 January 2005). Obstetrics and Gynecology Recall. Lippincott Williams & Wilkins. ISBN 9780781748797 – via Google Books.
- ^ a b A computer simulation run by Henri Leridon, PhD, an epidemiologist with the French Institute of Health and Medical Research:
- Leridon H (July 2004). "Can assisted reproduction technology compensate for the natural decline in fertility with age? A model assessment". Human Reproduction. 19 (7): 1548–1553. doi:10.1093/humrep/deh304. PMID 15205397.
- ^ Dunson DB, Baird DD, Colombo B (January 2004). "Increased infertility with age in men and women". Obstetrics and Gynecology. 103 (1): 51–56. doi:10.1097/01.AOG.0000100153.24061.45. PMID 14704244. S2CID 23061073.
- ^ Rothman KJ, Wise LA, Sørensen HT, Riis AH, Mikkelsen EM, Hatch EE (June 2013). "Volitional determinants and age-related decline in fecundability: a general population prospective cohort study in Denmark". Fertility and Sterility. 99 (7): 1958–1964. doi:10.1016/j.fertnstert.2013.02.040. PMC 3672329. PMID 23517858.
- ^ ASRM Practice Committee (September 2013). "Optimizing natural fertility: a committee opinion". Fertility and Sterility. 100 (3): 631–637. doi:10.1016/j.fertnstert.2013.07.011. PMID 23993665.
- ^ "Spanish woman 'is oldest mother'". BBC News. 2006-12-30. Retrieved 2006-12-30.
- ^ a b c Kidd SA, Eskenazi B, Wyrobek AJ (February 2001). "Effects of male age on semen quality and fertility: a review of the literature". Fertility and Sterility. 75 (2): 237–248. doi:10.1016/S0015-0282(00)01679-4. PMID 11172821.
- ^ Silber S (August 1991). "Effect of Age on Male Fertility". Seminars in Reproductive Medicine. 9 (3): 241–248. doi:10.1055/s-2007-1019415. S2CID 84196394.
- ^ Campagne DM (January 2013). "Can Male Fertility Be Improved Prior to Assisted Reproduction through The Control of Uncommonly Considered Factors?". International Journal of Fertility & Sterility. 6 (4): 214–223. PMC 3850314. PMID 24520443.
- ^ Wiener-Megnazi Z, Auslender R, Dirnfeld M (January 2012). "Advanced paternal age and reproductive outcome". Asian Journal of Andrology. 14 (1): 69–76. doi:10.1038/aja.2011.69. PMC 3735149. PMID 22157982.
- ^ Reichenberg A, Gross R, Weiser M, Bresnahan M, Silverman J, Harlap S, et al. (September 2006). "Advancing paternal age and autism". Archives of General Psychiatry. 63 (9): 1026–1032. doi:10.1001/archpsyc.63.9.1026. PMID 16953005.
- ^ Jaffe AE, Eaton WW, Straub RE, Marenco S, Weinberger DR (March 2014). "Paternal age, de novo mutations and schizophrenia". Molecular Psychiatry. 19 (3): 274–275. doi:10.1038/mp.2013.76. PMC 3929531. PMID 23752248.
- ^ Schulz SC, Green MF, Nelson KJ (1 April 2016). Schizophrenia and Psychotic Spectrum Disorders. Oxford University Press. ISBN 9780199378074 – via Google Books.
- ^ Malaspina D, Harlap S, Fennig S, Heiman D, Nahon D, Feldman D, Susser ES (April 2001). "Advancing paternal age and the risk of schizophrenia". Archives of General Psychiatry. 58 (4): 361–367. doi:10.1001/archpsyc.58.4.361. PMID 11296097.
- ^ Sipos A, Rasmussen F, Harrison G, Tynelius P, Lewis G, Leon DA, Gunnell D (November 2004). "Paternal age and schizophrenia: a population based cohort study". BMJ. 329 (7474): 1070. doi:10.1136/bmj.38243.672396.55. PMC 526116. PMID 15501901.
- ^ Malaspina D, Corcoran C, Fahim C, Berman A, Harkavy-Friedman J, Yale S, et al. (April 2002). "Paternal age and sporadic schizophrenia: evidence for de novo mutations". American Journal of Medical Genetics. 114 (3): 299–303. doi:10.1002/ajmg.1701. PMC 2982144. PMID 11920852.
- ^ "Obesity | Fat men linked to low fertility". Sydney Morning Herald. 18 October 2010. Retrieved 19 October 2010.
- ^ Plas E, Berger P, Hermann M, Pflüger H (August 2000). "Effects of aging on male fertility?". Experimental Gerontology. 35 (5): 543–551. doi:10.1016/S0531-5565(00)00120-0. PMID 10978677. S2CID 19875208.
- ^ Age Limit of Sperm Donors in the United Kingdom Pdf file Archived October 3, 2008, at the Wayback Machine
- ^ Arteaga O, Maoz BM, Nichols S, Markovich G, Kahr B (June 2014). "Complete polarimetry on the asymmetric transmission through subwavelength hole arrays". Optics Express. 22 (11): 13719–13732. doi:10.2307/286642. JSTOR 286642. PMID 24921565.
- ^ Pineau E (2020-01-23). "French Senate approves bill allowing IVF for single women, lesbians". Reuters. Retrieved 2021-04-21.
- ^ https://www.npr.org/2023/03/19/1163341684/south-korea-fertility-rate [bare URL]
- ^ Anderson, Thomas; Kohler, Hans-Peter (2013). "Education Fever and the East Asian Fertility Puzzle". Asian Population Studies. 9 (2): 196–215. doi:10.1080/17441730.2013.797293. PMC 4038909. PMID 24883076.
- ^ https://core.ac.uk/download/pdf/51182325.pdf [bare URL PDF]
- ^ Kim, Sunhye (2019). "Reproductive technologies as population control: How pronatalist policies harm reproductive health in South Korea". Sexual and Reproductive Health Matters. 27 (2): 6–12. doi:10.1080/26410397.2019.1610278. PMC 7888060. PMID 31533588.
- ^ "Vital Statistics of the United States 2003, Volume I, Natality", Table 1-1". Vital Statistics of the United States: 1980-2003. Centers for Disease Control and Prevention. 6 June 2019.
Live births, birth rates, and fertility rates, by race: United States, 1909-2003.
- ^ Oppenheimer VK. Women's rising employment and the future of the family in industrial societies. OCLC 936722012.
- ^ Bailey MJ (1 February 2006). "More Power to the Pill: The Impact of Contraceptive Freedom on Women's Life Cycle Labor Supply". The Quarterly Journal of Economics. 121 (1): 289–320. doi:10.1093/qje/121.1.289. hdl:1803/15760.
- ^ Sharma, Rakesh; Biedenharn, Kelly R; Fedor, Jennifer M; Agarwal, Ashok (2013-07-16). "Lifestyle factors and reproductive health: taking control of your fertility". Reproductive Biology and Endocrinology. 11 (1): 66. doi:10.1186/1477-7827-11-66. ISSN 1477-7827. PMC 3717046. PMID 23870423.
- ^ de Angelis, Cristina; Nardone, Antonio; Garifalos, Francesco; Pivonello, Claudia; Sansone, Andrea; Conforti, Alessandro; Di Dato, Carla; Sirico, Felice; Alviggi, Carlo; Isidori, Andrea; Colao, Annamaria; Pivonello, Rosario (2020-03-12). "Smoke, alcohol and drug addiction and female fertility". Reproductive Biology and Endocrinology. 18 (1): 21. doi:10.1186/s12958-020-0567-7. hdl:2108/272657. ISSN 1477-7827. PMC 7069005. PMID 32164734.
- ^ "Facts, Views and Vision in ObGyn". ObGyn. 15 (3). Universa BV. September 2023. doi:10.52054/fvvo.[full citation needed]
- ^ Makar RS, Toth TL (June 2002). "The evaluation of infertility". American Journal of Clinical Pathology. 117 (Suppl): S95-103. doi:10.1309/w8lj-k377-dhra-cp0b. PMID 14569805.
Further reading
This article incorporates material from the Citizendium article "Fertility (demography)", which is licensed under the Creative Commons Attribution-ShareAlike 3.0 Unported License but not under the GFDL.
- Barrett RE, Bogue DJ, Anderton DL (1997). The Population of the United States (3rd ed.).
- Bock J (March 2002). "Introduction: evolutionary theory and the search for a unified theory of fertility". American Journal of Human Biology. 14 (2): 145–148. doi:10.1002/ajhb.10039. PMID 11891930. S2CID 27386441.
- Campagne DM (January 2013). "Can Male Fertility Be Improved Prior to Assisted Reproduction through The Control of Uncommonly Considered Factors?". International Journal of Fertility & Sterility. 6 (4): 214–223. PMC 3850314. PMID 24520443.
- Chavarro J (2009). The Fertility Diet: Groundbreaking Research Reveals Natural Ways to Boost Ovulation and Improve Your Chances of Getting Pregnant. McGraw-Hill Professional. ISBN 978-0-07-162710-8.
- Coale AJ, Watkin SC, eds. (1986). The Decline of Fertility in Europe.
- Ehrhardt J, Kohli M, eds. (2011). "Special issue: Fertility in the History of the 20th Century: Trends, Theories, Policies, Discourses". Historical Social Research. 36 (2). Archived from the original on 2013-05-27.
- Eversley DE (1959). Social Theories of Fertility and the Malthusian Debate. Archived from the original on 2009-08-13. Retrieved 2017-08-27.
- Garrett E, Reid A, Schürer K, Szreter S (July 2001). Changing family size in England and Wales: Place, class and demography, 1891–1911. Cambridge University Press. Archived from the original on 2010-12-15. Retrieved 2017-08-27.
- Grabill WH, Kiser CV, Whelpton PK (1958). The Fertility of American Women. Archived from the original on 2009-08-13. Retrieved 2017-08-27.
- Guzmán J, Singh S, Rodríguez G, Pantelides E (1996). The fertility transition in Latin America. International Union for the Scientific Study of Population. Archived from the original on 2009-08-13. Retrieved 2017-08-27.
- Haines MR, Steckel RH, eds. (2000). A Population History of North America. Cambridge University Press.
- Hawes JM, Nybakken EI, eds. (1991). American Families: a Research Guide and Historical Handbook. Greenwood Press.
- Klein HS (2004). A Population History of the United States. Cambridge University Press.
- Knox PL, Bartels EH, Bohland JR, Holcomb B, Johnston RJ (2001). The United States: A Contemporary Human Geography. Longman UK/Wiley USA.
- Kohler HP (2001). Fertility and Social Interaction: An Economic Perspective. Archived from the original on 13 August 2009.
- Jones C (March 2008). "Ethical and legal conundrums of postmodern procreation". International Journal of Gynaecology and Obstetrics. 100 (3): 208–210. doi:10.1016/j.ijgo.2007.09.031. PMID 18062970. S2CID 13370582.
- Leete R (1999). Dynamics of Values in Fertility Change. Archived from the original on 13 August 2009.
- Lovett LL (2007). Conceiving the Future: Pronatalism, Reproduction, and the Family in the United States, 1890–1938.
- Mintz S, Kellogg S (1988). Domestic Revolutions: a Social History of American Family Life.
- Pampel FC, Peters HE (1995). "The Easterlin effect". Annual Review of Sociology. 21: 163–194. doi:10.1146/annurev.so.21.080195.001115. PMID 12291060.
- Population Handbook (5th ed.). Population Reference Bureau. 2004. Archived from the original on 2009-06-04.
- Reed J (1978). From Private Vice to Public Virtue: The Birth Control Movement and American Society Since 1830.
- Tarver JD (1996). The Demography of Africa. Archived from the original on 13 August 2009.
- Weeks JR (2007). Population: An Introduction to Concepts and Issues (10th ed.).
External links
- "Fertility treatment and clinics in the UK". Human Fertilisation and Embryology Authority (HFEA). Archived from the original on 2009-08-31.
- Population and the American future: the report. United States. Commission on Population Growth and the American Future. (Report). Washington: The Superintendent of Documents, U.S. Government Printing Office. 1972. hdl:2027/mdp.39015007261855.
- "United Nations World Population Prospects, the 2008 Revision". Archived from the original on 2010-07-09.
- Calder, Vanessa Brown, and Chelsea Follett (August 10, 2023). Freeing American Families: Reforms to Make Family Life Easier and More Affordable, Policy Analysis no. 955, Cato Institute, Washington, DC.

